"Anyone can experience an overdose and everyone is in a position to help."
Get the latest from Ken Warren straight to your inbox
Published Jan 02, 2025 • Last updated 0 minutes ago • 6 minute read

The numbers are as alarming as they are tragic.
From 2021 to 2023, there were 3,500 visits to emergency departments in Ottawa hospitals for opioid overdoses and 501 deaths.
In 2023 alone, 2,645 people died in Ontario from overdoses, 80 per cent of those cases associated with fentanyl.
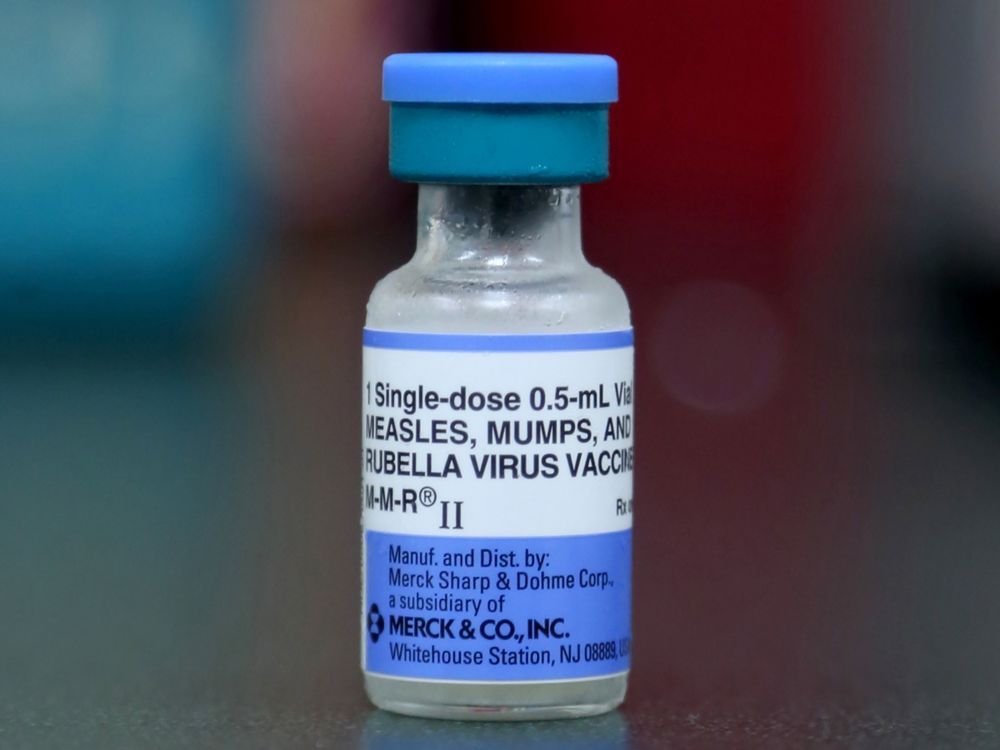
Accordingly, Ottawa Public Health is pushing a campaign to get naloxone — a medication that can reverse overdoses — into the hands of the public.
Advertisement 2
THIS CONTENT IS RESERVED FOR SUBSCRIBERS ONLY
Subscribe now to read the latest news in your city and across Canada.
- Exclusive articles from Elizabeth Payne, David Pugliese, Andrew Duffy, Bruce Deachman and others. Plus, food reviews and event listings in the weekly newsletter, Ottawa, Out of Office.
- Unlimited online access to Ottawa Citizen and 15 news sites with one account.
- Ottawa Citizen ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles, including the New York Times Crossword.
- Support local journalism.
SUBSCRIBE TO UNLOCK MORE ARTICLES
Subscribe now to read the latest news in your city and across Canada.
- Exclusive articles from Elizabeth Payne, David Pugliese, Andrew Duffy, Bruce Deachman and others. Plus, food reviews and event listings in the weekly newsletter, Ottawa, Out of Office.
- Unlimited online access to Ottawa Citizen and 15 news sites with one account.
- Ottawa Citizen ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles, including the New York Times Crossword.
- Support local journalism.
REGISTER / SIGN IN TO UNLOCK MORE ARTICLES
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account.
- Share your thoughts and join the conversation in the comments.
- Enjoy additional articles per month.
- Get email updates from your favourite authors.
THIS ARTICLE IS FREE TO READ REGISTER TO UNLOCK.
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account
- Share your thoughts and join the conversation in the comments
- Enjoy additional articles per month
- Get email updates from your favourite authors
Sign In or Create an Account
or
Article content
How to get training
Just like knowing CPR is an invaluable tool in an emergency, the goal is to have as many people as possible in a position to use naloxone to save friends, family members, neighbours or even strangers.
As part of an Ontario Ministry of Health mandate to address the crisis, naloxone (also known by the brand name Narcan) is free to everyone, available at a steadily growing number of pharmacies in the city.
OPH also offers training programs on how to use naloxone through its stopoverdoseottawa.ca website, which contains the sobering statistical truths surrounding the drug crisis.
“Anyone can experience an overdose and everyone is in a position to help,” said Harpreet Grewel, supervisor of Ottawa Public Health’s Addictions and Substance Use health team.
“We’re trying to get that information out to everyone. Taking these courses gives additional information on how to identify what an overdose looks like and what that response could look like.”
The programs also provide education aimed at altering some long-held views about drug users.
“It’s about how you can impact change,” Grewel said. “It addresses stigma related to people who use substances and mental health, the kind of stigma that can be a barrier for people to access services. We’ve come a long way, but we still have work to do.”
Advertisement 3
Article content
What’s the history of free over-the-counter naloxone kits in Canada?
Alberta was the first province to take the step, offering free kits at selected locations in 2015.
Health Canada made it a country-wide program in 2016 and the province launched the Ontario Naloxone Program for pharmacies, allowing them to offer free over-the-counter emergency kits.
How does someone find a pharmacy that carries naloxone?
The OPH website lists participating pharmacies, and residents can find one closest to them by inserting their postal code.
According to an Ontario Ministry of Health document updated in February 2024, two groups are eligible to receive the free kits: “an individual who is either at risk of currently using opioids or is a past user returning to opioid use” or “a family member or friend in position to assist an at-risk user.”
When the naloxone program was launched in 2016, a valid OHIP card was necessary to obtain the kits. That is no longer the case.
Individual pharmacists have discretion in determining whether kits should be made available.
“Pharmacists are expected to use their professional judgment when distributing kits and providing training,” the health ministry said.
By signing up you consent to receive the above newsletter from Postmedia Network Inc.
Article content
Advertisement 4
Article content
While there have been anecdotal reports of people being turned away, that comes as a surprise to Grewel.
“That’s so hard to hear,” she said. “We are really trying to create that community of compassion and normalizing the conversation about carrying naloxone, of stopping and helping your fellow neighbour, stranger or friend, anyone.”
What’s included with an emergency naloxone kit?
There are two types of kits.
One package includes a naloxone nasal spray (IN), which is sprayed directly into the nose. The other is a naloxone intramuscular injectible (IM). That’s a needle that is jabbed into the thigh, upper arm or buttocks.
Each kit contains how-to-use information, but pharmacists are also required to provide basic training information on how to use the naloxone.
“It’s really personal preference, which type of kit you choose to be trained in or to pick up,” said Megan Francoeur, a public health nurse with the OPH’s Addictions and Substance Use Health Team.
“We always recommend you call ahead to a pharmacy to make sure they have the (kit) you are looking for.”

How much do the naloxone kits cost the government?
Advertisement 5
Article content
The investment in saving lives comes at a cost.
After a pharmacy gives out a kit, it directly bills the Ontario government. The cost of an IM kit is $70, which includes the $35 kit itself, plus a $10 professional fee and the $25 training fee, according to the Ministry of Health. The cost for two kits is $70. (The training fee is removed if a recipient has previously completed a training course).
The cost of the IN nasal kit is $110, which includes a $10 professional fee.
What’s involved in the Ottawa Public Health training?
OPH recognizes that time is at a premium and the courses — including overdose prevention, response procedures and a “party safer” session — together take less than an hour.
“We also cover areas including being able to identify what an overdose is and calling 911,” Grewel said. “Getting someone the help they need when in distress is part of the response.”
The party safer session breaks down how the body reacts to a variety of substances.
“If someone chooses to use, it provides tips about how to use the drugs in a safer way,” Francoeur said. “The last bit of training is really educating people about where to get help and support for substances and to access mental health resources.”
Advertisement 6
Article content
What are the symptoms of an overdose?
Typically, signs of an overdose include shallow or slowed breathing, decreased consciousness and the appearance of pinpoint pupils. In some cases, there could be a blueing of the lips.
It should be noted that nausea, dizziness and/or a rapid heart rate are not generally considered symptoms of overdose. Those conditions are more likely associated with dehydration or heat-related injuries.
When in doubt about if there is an overdose, medical experts advise calling 911. Should a naloxone kit be available, it should be administered immediately. If naloxone is not available, listen closely to the advice from the emergency dispatcher.
What happens to the brain to cause a fentanyl overdose?
Fentanyl was originally marketed for its pain-killing prowess. The brain responds by releasing dopamine, which serves to deliver a feeling of euphoria.
The overwhelming power of fentanyl is that it also effectively changes breathing patterns, bypassing the opioid receptors that exist in the brainstem. It becomes overloaded with too many chemicals and the reflex action that normally controls breathing is turned off. Breathing can stop almost immediately.
Advertisement 7
Article content
Naloxone, originally patented in 1961, can counter those effects.
In some cases, it could take as many as four doses of naloxone for a patient to fully recover from an overdose. Canadian hospitals have been routinely using naloxone to treat patients for 50 years.
What legal protection exists for people who use naloxone in an emergency?
Recognizing the dangers of the growing drug epidemic and encouraging the emergency use of first aid in crisis situations, both the federal and provincial governments have shielded those asking for emergency services from police charges.
The federal Good Samaritan Drug Overdose Act, enacted in 2017, “protects people from charges of possession of illegal drugs and probation orders,” according to Kevin Butler, a lawyer at Ottawa law firm Tierney and Stauffer.
That law doesn’t extend to offences including outstanding warrants or the production and/or trafficking of illegal substances.
Ontario’s Good Samaritan Act, which came into effect in 2001, is about civil protection for anyone who acts quickly to a vital medical issue. “That legislation applies to someone who provides emergency first aid,” Butler said.
Advertisement 8
Article content
Is Naloxone used at the city’s safe consumption sites?
Yes. While the very notion of approved sites is a needlepoint of contention, trained professionals are on site to handle crisis situations at the four emergency locations in Ottawa.
Those include The Trailer at the Shepherds of Good Hope at 230 Murray St., Ottawa Public Health’s headquarters at 179 Clarence St., the Sandy Hill Community Centre at 221 Nelson St. and the Somerset West Community Health Centre at 55 Eccles St.
The Somerset West location is scheduled to close in April 2025 because the Ontario government has ruled its proximity to a nearby school represents a hazard.
According to OPH, there had been 18,700 visits to those sites in 2024 as of mid-November. In the past three years, there have been more than 4,700 overdoses reported, with naloxone required in 3,031 cases. There had been no deaths.
Our website is your destination for up-to-the-minute news, so make sure to bookmark our homepage and sign up for our newsletters so we can keep you informed.
Recommended from Editorial
-

What it's like helping those on fentanyl in the ByWard Market
-

Ottawa's death toll from drug overdoses appears headed for record in 2024
Article content
.png)
 2 days ago
8
2 days ago
8
































 Bengali (BD) ·
Bengali (BD) ·  English (US) ·
English (US) ·