The safer supply program, which hands out high-doses of opioids and stimulants to protect drug users, is about to lose federal funding.
Published Dec 30, 2024 • Last updated 0 minutes ago • 9 minute read

Four years ago, the opioid epidemic was brought to the doorstep of Steve’s Music Store when an addictions clinic, Recovery Care, and a specialized pharmacy, Respect RX, opened next door.
Both are part of Ottawa’s experiment in safer supply – a program that sees hundreds of people who use drugs prescribed high doses of medical-grade opioids or stimulants to protect them from contaminated street drugs.
Advertisement 2
THIS CONTENT IS RESERVED FOR SUBSCRIBERS ONLY
Subscribe now to read the latest news in your city and across Canada.
- Exclusive articles from Elizabeth Payne, David Pugliese, Andrew Duffy, Bruce Deachman and others. Plus, food reviews and event listings in the weekly newsletter, Ottawa, Out of Office.
- Unlimited online access to Ottawa Citizen and 15 news sites with one account.
- Ottawa Citizen ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles, including the New York Times Crossword.
- Support local journalism.
SUBSCRIBE TO UNLOCK MORE ARTICLES
Subscribe now to read the latest news in your city and across Canada.
- Exclusive articles from Elizabeth Payne, David Pugliese, Andrew Duffy, Bruce Deachman and others. Plus, food reviews and event listings in the weekly newsletter, Ottawa, Out of Office.
- Unlimited online access to Ottawa Citizen and 15 news sites with one account.
- Ottawa Citizen ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles, including the New York Times Crossword.
- Support local journalism.
REGISTER / SIGN IN TO UNLOCK MORE ARTICLES
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account.
- Share your thoughts and join the conversation in the comments.
- Enjoy additional articles per month.
- Get email updates from your favourite authors.
THIS ARTICLE IS FREE TO READ REGISTER TO UNLOCK.
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account
- Share your thoughts and join the conversation in the comments
- Enjoy additional articles per month
- Get email updates from your favourite authors
Sign In or Create an Account
or
Article content
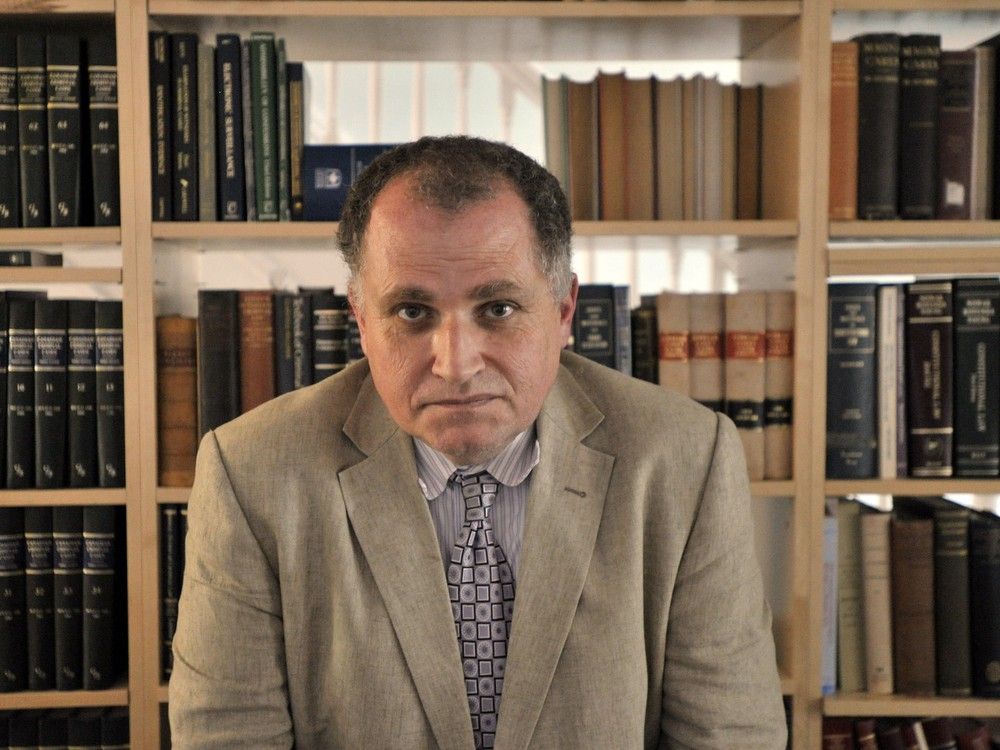
Steve’s Music Store manager Dan Sauvé says the program gave birth to a “criminal ecosystem” that preyed on safe supply clients, and led to more theft, drug dealing and unpredictable behaviour on Rideau Street. The store locked its front door, and allowed customers in one by one.
When the lease came up for renewal last month, Steve’s owners made the difficult decision to move from the Rideau Street location they’ve occupied for 42 years. The social chaos that came with safe supply was the final straw.
“To me,” Sauvé says, “the question is: How can we help people without causing so much collateral damage to neighbourhoods?”

Delivered by an organization called Safer Supply Ottawa, the city’s four-year-old pilot program now serves about 500 people who use drugs.
Its proponents contend the program saves lives, but with federal funding about to expire in March 2025, its future is in serious doubt: The Ontario government has made plain it doesn’t want anything to do with safer supply.
“As far as I’m concerned the federal government is the biggest drug dealer in the entire country,” Premier Doug Ford charged earlier this year. “It’s unacceptable, it needs to stop. We need to get rid of safe supply and put money into treatment and detox beds. That’s what we need to do, not continue to give people free drugs.”
Advertisement 3
Article content
In November, the Ford government tabled a bill, the Safer Streets, Stronger Communities Act, that will require municipalities to obtain provincial approval before taking part in a federally-funded safer supply program.
It has thrust safer supply, also known as prescribed alternatives, to the centre of a highly polarized debate. While Ford and other critics contend safer supply is part of the problem – increasing the overall supply of opioids – others hold it up as a life-saving part of the solution: the best way to reduce the death toll from toxic street drugs.
“The problem is the toxic drug crisis,” argues Donna Sarrazin, chief executive officer of Recovery Care, an Ottawa firm that operates five drug treatment clinics in the region, and offers prescribing services for Safer Supply Ottawa.
“Safer supply helps to keep individuals alive while also offering them additional supportive services and engagement opportunities. You can’t recover from addiction if you are dead.”
Safer Supply Ottawa was launched in July 2020 with a five-year, $9.6 million federal grant. Its mandate: to expand the prescription of pharmaceutical opioids to drug users who face the greatest risk of overdose and death. The federal money paid mostly for additional “wrap-around services” such as primary health care, housing support, case management, counselling and mental health services.
By signing up you consent to receive the above newsletter from Postmedia Network Inc.
Article content
Advertisement 4
Article content
Sarrazin insists the end of federal funding in March will not spell the end of the program since willing doctors and nurse practitioners will still be able to prescribe opioids and stimulants to drug-addicted patients.
Ontario Works and the Ontario Disability Support Program cover the cost of most prescription medications.
“At this time, there is no mechanism in place that prevents any prescriber from prescribing in this format,” says Sarrazin, program lead for Safer Supply Ottawa. “It’s unclear what changes the Ford government could or would make that could impact this ability.”
Hannah Jensen, director of communications for Health Minister Sylvia Jones, did not respond to a question about whether safer supply prescribing is an issue for the Ford government.
It means the heated debate about the future of safer supply will continue even as key research questions remain unanswered.
***

Safer Supply Ottawa was introduced as the COVID-19 pandemic compounded the pain, isolation and risk faced by drug users, many of them homeless. The pandemic’s travel restrictions also disrupted conventional drug supply routes so Canadian cities were flooded with drugs concocted in basement chemical labs.
Advertisement 5
Article content
In Ottawa, overdoses appeared in clusters, driven by the toxicity of the new supply.
Safer supply was a harm reduction measure born of desperation: a way to save people from the dangerous and unpredictable drugs being sold on city streets.
A coalition of frontline health care agencies came together to manage the program: Pathways to Recovery, Recovery Care, Respect Rx Pharmacy, Ottawa Inner City Health, Options Bytown, Sandy Hill Community Health Centre, Somerset West Community Health Centre and Ottawa Public Health.
Three of those agencies, Recovery Care, Ottawa Inner City Health, and Somerset West Community Health Centre, offered prescribing services.
The Ottawa Safer Supply program was designed with as “few barriers as possible” for users. It offers flexible eligibility requirements and unobserved dosing, which means participants can leave with their opioids or stimulants in hand to administer on their own.
The approach was designed to allow users to medicate their drug cravings without having to repeatedly return to a pharmacy.
Prescribers in the program typically offer clients short-acting hydromorphone (Dilaudid) tablets to control drug cravings, along with a long-acting opioid such as methadone or slow-release oral morphine. The drugs are meant to replace fentanyl and its analogues.
Advertisement 6
Article content
Up to 240 mg of daily hydromorphone can be prescribed for each client. (Dilaudid’s manufacturer, Purdue Pharma, recommends a daily maximum dose of 18 mg for chronic pain.)
Those in the safer stimulant program typically receive short-acting methylphenidate, along with a long-acting version of the same drug, or dextroamphetamine. The prescribed stimulants, commonly used to treat ADHD, are meant to replace street drugs such as crystal meth and crack cocaine.
According to a recently published study on Ottawa’s safer supply program conducted by University of Ottawa researchers, 70 per cent of those in the opioid replacement program said they used less fentanyl during the four-month study period (Aug. 1 – Nov. 30, 2023). Among those receiving medical grade stimulants, 67 per cent reported using less from the unregulated drug market.
Among those receiving both safer opioids and stimulants, 66 per cent reported using less fentanyl and 63 per cent said they used fewer stimulants.
More than three-quarters of all participants (77 per cent) did not report a drug overdose during the four-month study period.
Advertisement 7
Article content
The study was based on self-reporting by clients.
At the time of the study, 470 people were enrolled in the safer supply program: 244 received medical-grade opioids, 36 received stimulants and 190 received both.
The study, one of four that examined the program, does not address some important questions. None of the evaluation studies tracked how many clients died, were hospitalized, or pursued drug rehab during the first four years of the safer supply program. There was also no control group for comparison purposes.
As part of the April 2023 study, researchers asked a select group of safer supply clients about diversion: the extent to which prescribed drugs were gifted, traded or sold to people outside the program. Most acknowledged that diversion did occur.
Some participants told researchers that people trade Dilaudid for fentanyl because the latter drug is more potent.
In a webinar, lead researcher Marlene Haines said some participants gave away drugs because of concern for the health of loved ones not in the program, or to help friends going through withdrawal.
Advertisement 8
Article content
“If we look at the culture of people who use drugs, they have always shared and have always taken care of one another, especially considering how rejected many of them feel and marginalized,” she said.
Haines declined an interview request for this story. The Ottawa Police Service referred questions about diversion to Ottawa Public Heath, which in turn referred questions to Sarrazin.
Sarrazin concedes that diversion is a challenge in safer supply, but she contends it’s an issue with all prescription services, and with conventional addiction treatment, known as opioid agonist treatment. (It uses medications such as buprenorphine, methadone and Suboxone to treat drug addiction.)
“Diversion didn’t start with the introduction of prescribed alternatives,” she says.
British Columbia has the most experience with safer supply. In March 2020, B.C. rolled out the country’s first province-wide safer supply program: It allowed doctors and nurse practitioners to prescribe free pharmaceutical-grade opioids to people at high risk of overdose.
Earlier this year, provincial health officer Dr. Bonnie Henry issued a report on the program that called for its expansion to rural and remote communities, but the idea was rejected by the B.C. government. More than 4,300 people in the province receive opioids and/ or stimulants under the existing program.
Advertisement 9
Article content
Vancouver Deputy Police Chief Fiona Wilson told a Commons committee in April that about 50 per cent of hydromorphone seizures in the province came from safer supply diversions.
But there’s also some research that suggests the B.C. program is saving lives. A study published early this year in the British Medical Journal found people in the opioid safer supply program were significantly less likely to die in the week after filling an opioid prescription than users who did not have access to the program. The study did not find the same benefit for people receiving prescribed stimulants.
Safer supply is controversial even among doctors who treat people with addictions. Dr. Vincent Lam, a Toronto addictions specialist and author who has written extensively about the opioid crisis, has said he opposes safer supply because, as a physician, he’s committed to the ethical principle ‘do no harm.’
Prescribing high doses of short-acting hydromorphone increases individual opioid tolerance levels, he said, while also adding to the overall supply of opioids on city streets.
Advertisement 10
Article content
“The more they (short-acting opioids) are used, the less effective they are, requiring ever higher doses, higher potencies, and entailing greater risks of overdose and death,” he wrote.
Most researchers trace the start of the current opioid epidemic to the late 1990s when OxyContin was heavily marketed by its manufacturer, Purdue Pharma, and widely prescribed to people in search of pain relief.
“Prescribed opioids were an integral part of the creation of this crisis,” Lam argued. “We are not going to be able to prescribe our way out of it.”
****

In Ottawa, there has been no public reporting of the extent to which prescription drugs have been “diverted” onto the street, and to whom. Similarly, there’s no understanding as to whether the program has reduced the overall demand for fentanyl and other opioids.
What is known is that the number of confirmed overdose deaths has increased in Ottawa in each of the past four years.
Rideau-Vanier Coun. Stéphanie Plante, whose ward encompasses the ByWard Market and Sandy Hill, says she’s not opposed to safer supply when prescribed opioids or stimulants are consumed in front of a doctor or nurse. But she contends the existing system is widening the city’s opioid epidemic.
Advertisement 11
Article content
“I think this model is absolutely not working,” she says. “We find pill bottles all the time in my ward.”
Plante contends the program should have been intensively studied before it was expanded. Instead, she says, the program moved ahead with little or no research into downside risks, and with little or no consultation with local residents and businesses.
Calla Barnett, chair of Action Sandy Hill’s community and social services committee, says she supported the idea of safer supply when it was first introduced. But during the past four years, Barnett says, she has become convinced the program is now part of the problem.
“What it has meant is an increase in drug use,” she charged. “Dilaudid, hydromorphone have become a kind of currency. They’re tradeable for food or fentanyl.”
In early December, Ontario Auditor General Shelley Spence’s report on Ontario’s opioid strategy called it both outdated and ineffective. The report, among other things, looked at the use of safer supply in Ontario.
Based on its data analysis, the office of the auditor general estimated that the safer supply dispensing of hydromorphone in Ontario increased by 251 per cent between 2019-20 and 2023-24. It now accounts for an estimated 686,000 hydromorphone doses dispensed in the province.
Advertisement 12
Article content
The auditor general noted the Ministry of Health “has not taken any action to evaluate the extent of safer opioid supply’s adoption, as well as its effectiveness and outcomes.”
Spence recommended the ministry conduct that research to allow for evidence-informed decisions about the program’s future in Ontario.
Our website is your destination for up-to-the-minute news, so make sure to bookmark our homepage and sign up for our newsletters so we can keep you informed.
Recommended from Editorial
-

Victim of Christmas Day homicide remembered as 'a beautiful person'
-

Remembering 17 remarkable Ottawans who died in 2024
Article content
.png)
 1 week ago
15
1 week ago
15
































 Bengali (BD) ·
Bengali (BD) ·  English (US) ·
English (US) ·